Problems We Solve
Employer-sponsored health insurance covers 153-Million non-elderly people. If you are frustrated with the rising cost of employer sponsored health benefits and feel that your plan is not effectively addressing the needs of your workforce, you’re not alone.
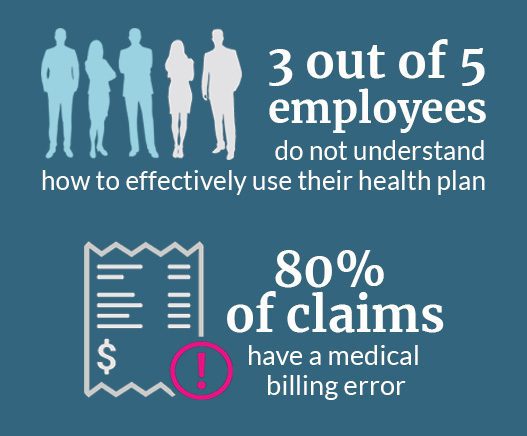
Recent government data estimates that people in the United States owe at least $220 billion in medical debt. Despite recent regulatory changes there has been little to address how employers effectively address this challenge. Employers have no choice by to turn to increasing premiums that lead to reduced benefits or higher out-of-pocket costs passed on to employees.
My Medical Navigator takes an integrated approach when helping employers and their employees navigate their way through understanding plan performance and reducing healthcare waste. Our unique combination of decades of healthcare advocacy experience and our best-in-class technology will transform how you offer and utilize your medical benefits.
How Your Organization Will Benefit from Using My Medical Navigator
-
Cost containment solutions that are seamless and effective.
MMN’s AI platform Claimlytic™ and associated tools, delivers healthcare price transparency, real-time benefit accumulators and, benefit insights in seconds.
-
Claim audits ensure you do not overpay for inaccurate bills.
-
Overpayment recovery ensures carrier payments are aligned with contract terms.
How Your Employees Will Benefit from Using My Medical Navigator
- Employees have access to their own personal Navigator at any point in their healthcare journey.
- A mobile app using the power of AI, MyMedicalShopper™ enables employees to make informed decisions about how and where they select providers and how their choices align with their benefit plan.
- Out-of-pocket expenses will be reduced by an average of 30%.
- Complex claim issues are handled by a knowledgeable Navigator. Allowing employees to focus on healing and not administrative headaches.

